Cognitive behavioral therapy (CBT) is widely regarded as the leading approach for treating various mental health conditions, supported by decades of empirical evidence.
But how effective are CBT principles in addressing the distress stemming from an uncontrollable urge to daydream?
While maladaptive daydreaming (MD) isn’t formally acknowledged as a mental health disorder, the compulsive urge to indulge in extensive fantasy daydreams severely impacts individuals suffering from it.
Research into CBT for maladaptive daydreaming is still emerging, but some interesting results have already been found. Here’s where the evidence stands currently.
BetterHelp has over 30,000 licensed therapists, many of which practice cognitive behavioral therapy and can assist with maladaptive coping mechanisms. Prices starting at $65/week. To get started with BetterHelp online therapy, click here to fill in their brief questionnaire. Discussing Psychology readers get 15% off their first month with BetterHelp.
Cognitive Behavioral Therapy for Maladaptive Daydreaming
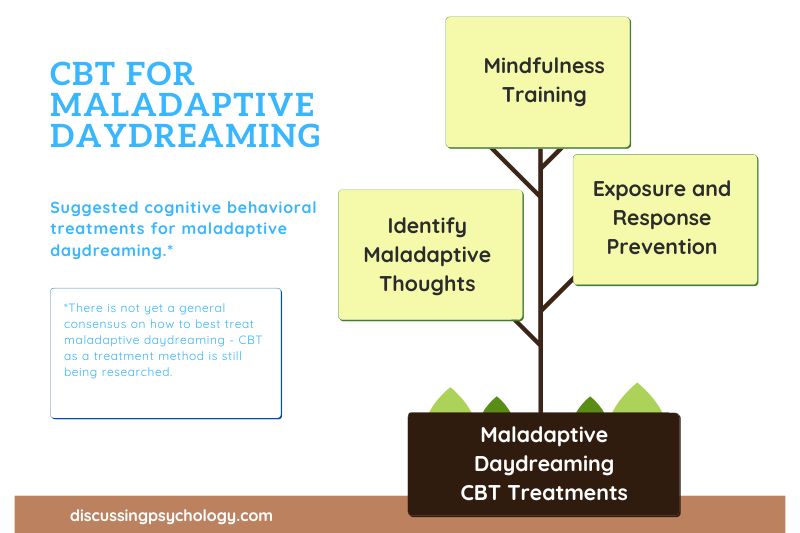
Early research suggests that a combination of mindfulness training, cognitive restructuring, and strategies used to treat addictions can significantly reduce the distress MD causes.
Part of the problem with diagnosing and treating maladaptive daydreaming is that there’s still so much we don’t know about it.
MD shares a lot of similarities, symptoms, and risk factors with various other psychological conditions, including
- Dissociative disorders: Conditions involving detachment from reality.
- Addictions: MD is often described as producing an extreme yearning to spend time daydreaming, similar to an addiction.
- Compulsions: The meticulous, detailed nature of daydreams and strong compulsions to spend time in them could alternatively be likened to the compulsions in conditions such as OCD.
- Attention-related disorders: The inability to control one’s thoughts present in MD is highly reminiscent of attention problems, such as ADHD.
- Social impairment: MD has been linked to social anxiety in that those with MD are often highly isolated and lonely.
- Trauma response: Research suggests a strong link between childhood trauma and maladaptive daydreaming in later life
Related: Our free online maladaptive daydreaming quiz is based on the original 16-item maladaptive daydreaming scale which aims to identify traits of MD.
Difficulty Selecting Treatments
The multifaceted nature of MD means that there is currently no consensus on how exactly the disorder should be treated.
Should MD be considered an addiction and treated in line with other forms of non-chemical addiction?
Is it primarily a response to adverse experiences best treated using a trauma recovery framework?
Or would treating the social or attention impairments be the most effective way to relieve symptoms?
Time and further research will tell what the most effective framework for MD treatment using CBT is.
Until then, there have been several small-scale case studies of treatment for maladaptive daydreaming using a combination of the above rationales, with promising results.
Treating Maladaptive Daydreaming as an Addiction
Two case studies from 2018 and 2019 described combatting MD using behavioral methods designed to treat addictions.
The goal was not to totally eliminate daydreaming from the patient’s lives, since everyone daydreams to an extent, but rather to limit and control daydreaming until it no longer causes such significant impairment.
Methods employed include:
- Identifying and avoiding triggers which lead to the onset of MD.
- Creating a daily schedule of activity, thereby reducing the temptation to spend time daydreaming.
- Allocating a single period in the evening in which the patient was allowed to daydream.
- Employing positive reinforcement and self-rewards for meeting goals such as successfully noticing the onset of daydreaming and pulling oneself out.
- Maintaining accountability to others in regard to time spent daydreaming.
- Developing positive affirmations to remind oneself of the harmful effects of daydreaming when one feels tempted (such as ‘daydreaming is harmful to me’ or ‘I will deal with my distress in the present rather than escape into a future fantasy’).
This methodology was found to be effective in both patients after a period of treatment lasting several months.
One patient reported that his time spent in daydreams was reduced down from several hours to just 15 minutes per day, while the other reported a 50% reduction in MD time and a 70% increase in his level of adjustment to normal life.
Other treatment approaches
Incorporating other elements into treatment may lead to greater gains. Some possible avenues to explore include the following:
Maladaptive thoughts
One of the core principles of cognitive behavioral therapy is that adverse experiences lead to us viewing the world in a negative, distorted way. These maladaptive thoughts then lead us to feel distress and to act in unhelpful ways.
Applying this to maladaptive daydreaming, a person who has experienced childhood trauma or who is finding life challenging and unrewarding in the present may develop maladaptive ways of thinking and turn to fantasies as a way of coping with the distress they cause.
Through a process called cognitive restructuring, CBT teaches patients to identify and disrupt these negative thoughts by treating them as hypotheses to test rather than as hard facts.
Once a patient has developed a more realistic, less harmful way of thinking, their level of distress decreases and the need to escape into daydreams vanishes.
Exposure and Response Prevention (ERP)
A rather drastic form of treatment, it takes its cues from ERP, a CBT method designed to treat OCD by exposing the patient to situations in which they normally feel the need to act compulsively and trains them not to act compulsively.
In the case of MD, patients are training not to engage in daydreams by deliberately making them less pleasant.
This could involve changing the story to be more negative, killing characters or finding other ways to make the fantasy an unappealing place to spend time.
While this method has the potential to be effective, bringing their years-long fantasies to an abrupt and painful end might be a tough sell for many MD patients given the pleasure they take from their fantasies.
Furthermore, if MD is considered a coping mechanism to help people respond to trauma and unmet needs, denying them this coping mechanism without teaching other, more effective ways of managing stress could be seen as comparable to throwing them out of a plane without a parachute.
It’s worth noting that ERP is typically most effective when guided by a licensed therapist.
Online therapy platforms such as SonderMind or BetterHelp are great ways to connect with mental health professionals. However, you can also seek CBT/ERP treatment from traditional in-person private therapy clinics if that is your preference.
Mindfulness training
If MD is the practice of coping with distress by shifting your attention onto fantasies, mindfulness helps you achieve the same goal by turning your focus to the present moment.
Mindfulness meditation is used in CBT to help patients disengage from their maladaptive thoughts, rather than feeling the need to follow through on them.
For patients with MD, this helps create some distance between the person and the urge to daydream, helping reduce mind wandering, improve attention, and make it easier to ignore the temptation to daydream.
Help is available
While finding a CBT therapist who is familiar with MD may not always be possible, any qualified therapist would be able to recognize the emotional distress, negative patterns of thought and behavior, and overall life impairment of a patient with MD who came to them and would be able to develop an appropriate treatment plan.
So if daydreaming has turned your life into a nightmare, speak to a qualified therapist, tell them about what you’re going through, and find out how they can help.
BetterHelp has over 30,000 licensed therapists, many of which practice cognitive behavioral therapy and can assist with maladaptive coping mechanisms.
Prices starting at $65/week. To get started with BetterHelp online therapy, click here to fill in their brief questionnaire.
- Rebello, P., Johnson, K., D’Souza, P., Rao, P. P., & Malarmathi, M. S (2019). A case report on maladaptive daydreaming. Galore International Journal of Health Sciences and Research, 4(1). https://www.gijhsr.com/GIJHSR_Vol.4_Issue.1_Jan2019/7.pdf
- Ross, C., Ridgway, J., & George, N. (2020). Maladaptive daydreaming, dissociation, and the dissociative disorders. Psychiatric Research and Clinical Practice, 2(2), 53–61. https://doi.org/10.1176/appi.prcp.20190050
- Soffer-Dudek, N., & Somer, E. (2018). Trapped in a daydream: Daily elevations in maladaptive daydreaming are associated with daily psychopathological symptoms. Frontiers In Psychiatry, 9. https://doi.org/10.3389/fpsyt.2018.00194
- Somer, E. (2018). Maladaptive daydreaming: Ontological analysis, treatment rationale; a pilot case report. Frontiers in the Psychotherapy of Trauma and Dissociation, 1, 1-22. https://www.researchgate.net/publication/322152657_Maladaptive_Daydreaming_Ontological_Analysis_Treatment_Rationale_a_Pilot_Case_Report
- Somer, E., Abu-Rayya, H., & Brenner, R. (2020). Childhood trauma and maladaptive daydreaming: Fantasy functions and themes in a multi-country sample. Journal of Trauma & Dissociation, 22(3), 288–303. https://doi.org/10.1080/15299732.2020.1809599
- Somer, E., & Herscu, O. (2017). Childhood trauma, social anxiety, absorption and fantasy dependence: Two potential mediated pathways to maladaptive daydreaming. Journal of Addictive Behaviors,Therapy & Rehabilitation, 06(04). https://doi.org/10.4172/2324-9005.1000170
- White, M. A. (2021, November 30). Maladaptive daydreaming. Healthline. https://www.healthline.com/health/mental-health/maladaptive-daydreaming